POSTERIOR CRUCIATE LIGAMENT (PCL)
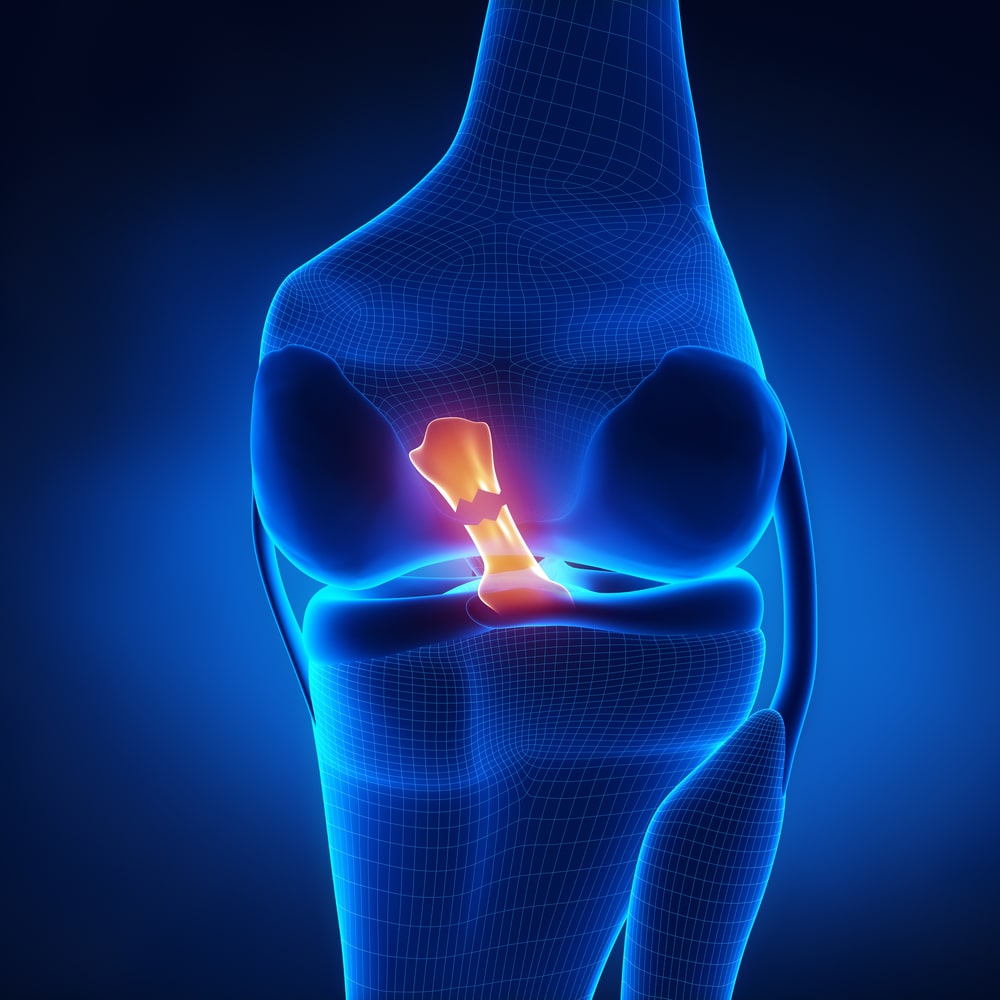
POSTERIOR CRUCIATE LIGAMENT (PCL) SURGERY
Posterior Cruciate Ligament (PCL) Surgery is a reconstructive procedure aimed at repairing or replacing a torn PCL, which is responsible for stabilizing the knee by preventing the tibia from sliding backward relative to the femur. PCL injuries often occur in high-impact sports or through direct trauma to the knee. The surgery typically involves using a graft (autograft or allograft) to replace the damaged ligament, and is generally performed arthroscopically for minimally invasive access. Post-surgery, a structured rehabilitation program focusing on strength, mobility, and knee stability is essential for a successful recovery and return to activity. Recovery time varies, but athletes may return to sports after 6-12 months, depending on the extent of the injury and surgical outcome.
- Flexible and fast scheduling
- Regular quality assurance
Here’s how it works:
Diagnosis and Preoperative Evaluation
The process begins with clinical examination and imaging (MRI, X-ray) to confirm the extent of the PCL injury and assess any associated damage to other knee structures.
Anesthesia Administration
The patient is administered regional or general anesthesia to ensure a pain-free procedure and facilitate a controlled surgical environment.
Arthroscopic Assessment
A minimally invasive arthroscope is inserted into the knee to visualize the joint, confirm the diagnosis, and evaluate surrounding ligaments, cartilage, and menisci.
Post-Surgery Care:
The knee is bandaged, and sometimes a brace is applied to protect the joint. Pain management and swelling control are critical in the immediate post-operative period. The patient may be given crutches to avoid putting weight on the knee.
Graft Selection and Preparation
A tendon graft, either autograft (from the patient) or allograft (donor tissue), is selected and prepared to replace the torn PCL, ensuring biomechanical strength and compatibility.
Tibial and Femoral Tunnel Drilling
Precision-guided tunnels are drilled in the tibia and femur to anchor the graft in anatomical alignment, mimicking the natural course of the PCL.
Graft Insertion and Fixation
The graft is carefully inserted through the drilled tunnels and securely fixed using screws or buttons to maintain tension and proper alignment within the knee joint.
Closure and Recovery Protocol
Surgical incisions are closed, and a structured rehabilitation program is initiated post-surgery to restore knee function, strengthen surrounding muscles, and prevent stiffness.
Posterior Cruciate Ligament (PCL) Surgery is commonly used for conditions like

Dashboard Injury (Trauma from Car Accidents)
– A sudden impact to the front of the knee, often seen in car collisions, forces the tibia backward and tears the PCL, frequently requiring surgical intervention due to complete rupture.

Associated Meniscal or Cartilage Damage
– PCL injuries often coincide with meniscus tears or cartilage degeneration, which, when combined, warrant surgical treatment to repair all damaged structures and prevent further joint deterioration.

Complete (Grade III) PCL Ruptures
– In severe cases where the PCL is entirely torn, the ligament does not heal effectively on its own, making surgical repair or reconstruction essential for joint stabilization and long-term mobility.

Chronic PCL Deficiency
– Untreated or inadequately managed PCL injuries can lead to ongoing knee instability, pain, and limited function, ultimately requiring surgery to restore biomechanical integrity.

Multiligament Knee Injuries
– PCL tears occurring alongside injuries to the ACL, MCL, or lateral structures result in major joint instability, necessitating complex surgical reconstruction to restore full knee function.

Sports Injuries
– High-impact or contact sports such as football, rugby, or skiing can cause hyperextension or twisting injuries that lead to partial or full-thickness PCL tears, especially in athletes requiring high performance levels.
